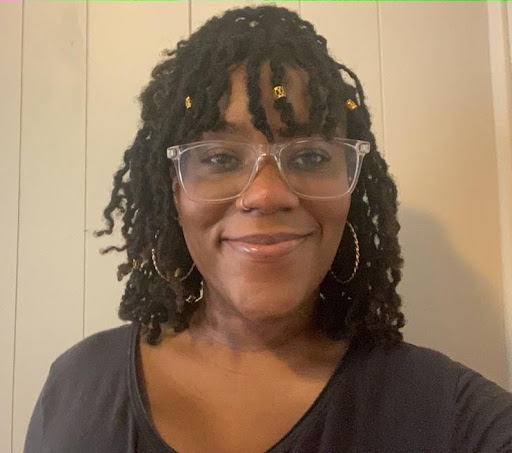
Michaela Harris is a second-year MPH candidate at Boston University School of Public Health specializing in Global Health Program Design, Monitoring, and Evaluation with a concentration in Maternal and Child Health. Outside of her work as a Health Promotion Advocate, Michaela works part-time as a research assistant in the Division of Women’s Health at Brigham and Women’s Hospital involved in trauma informed care (TIC) initiatives. Michaela’s public health interests include respectful maternity care, access and quality care initiatives, ACEs, and reproductive justice (internationally and abroad). After graduation, Michaela will continue her work in trauma-informed care projects especially tailored to the maternal and child health population, while strengthening her application for medical school.

Melanie Lambert is a second-year MPH candidate at Boston University School of Public Health concentrating in Community Assessment, Program Design, Implementation, and Evaluation, as well as Maternal and Child Health. Aside from her work as a health promotion advocate, Melanie also serves as the co-president of BUSPH’s Period Project, a group that aims to get menstrual products on campus as well as working towards menstrual equity within the greater Boston community. In addition to her graduate studies, Melanie works part time in Mass General’s Gastroenterology Department as a quality and safety data analyst. Melanie’s public health interests include adolescent health promotion, menstrual equity, quality improvement for health programs, and respectful care for birthing individuals. After graduation, Melanie would like to apply to medical school where she hopes to utilize her public health training to advance the health of her future patients.
In December 2020, we had the opportunity to embark on a wonderful project. Through the Boston University School of Public Health Maternal and Child Health Center of Excellence we became Practice Fellows in the Health Promotion Advocacy Program (HPAP) at Boston Medical Center’s (BMC) Pediatric Emergency Department.
Communication
Under the direction of Drs. Edward Bernstein and Sadiqa Kendi, this opportunity allowed us to craft a survey that we would use to screen patients from the ages of 13-23, ascertaining the various social determinants that may be impacting their health. It also allowed us to utilize Brief Negotiated Interviewing (BNI) to encourage behavioral change. Most importantly, we were given the privilege to learn about patients and to hear their stories. Throughout our fellowship, we have met so many beautiful souls from various walks of life that trusted us enough to share themselves and allow us to provide whatever support we could.
An important aspect of our fellowship was communication, both to our interdisciplinary team of healthcare professionals and patients. We had weekly meetings with our preceptor where we shared what we learned and were given feedback on our progress. We also met with many different individuals throughout the Boston and BMC communities to share how we could collaborate to make our program better, and to learn about the various resources that we could provide to patients.
Communication was also vital when interacting with patients. We initially approached our first shift in the ED with some anxiety, afraid that we wouldn’t be good enough. However, upon walking into the first patient’s room we saw some of the stress they had been carrying leave their body- a nonverbal cue that they were relieved to have hospital personnel that they could identify with and who were eager to hear their story and provide help. Throughout our time we have had conversations with patients about mental health, sexual health, alcohol, tobacco, and other drug usages, and COVID-19. We were amazed at the impactful conversations we had surrounding all of these topics, but especially COVID-19 vaccination. We were able to create a safe space for patients to express their concerns without judgment. Patients were excited to share their opinions and wanted to hear the firsthand experiences of two Black women that decided to get vaccinated. Respectful communication allowed us to help several young people decide for themselves to get vaccinated.
Increasing the knowledge of health resources available to our patients was another top priority for us, and one of the most impactful tools we’ve used is the THRIVE database (in conjunction with our assessment). This tool allowed us to create customized referrals to community resources based on the patient’s zip code, ensuring that the resources provided were within a reasonable distance to their respective communities. We also had the option of sending referrals inside of the tool or to the patient directly in a variety of different languages. This database allowed us to communicate available resources to our patients, not just within Boston Medical Center, but throughout the Greater Boston community in a way that was accessible to them.
MCH Knowledge
In addition to strengthening MCH Competency 5, we also gained knowledge in many areas of Maternal and Child Health. As Health Promotion Advocates, we had plenty of opportunities to collaborate with and learn from various departments within the Boston Medical Center community, including their addiction help services through Projects ASSERT and CATALYST and violence prevention services delivered by their Violence Intervention Advocacy Program (VIAP). We also strengthened our MCH Knowledge through other programs such as the BMC Food Pantry, and the Adolescent Sexual Health Clinic. In addition, this program allowed us to become well versed in the SBIRT Framework (Screening, Brief Intervention, and Referral to Treatment), which enabled us to assess the severity of the patient’s health behaviors (i.e substance misuse, sexual health practices, etc) while putting the patient in the driver’s seat to cultivate self-awareness and develop an action plan as needed. It’s one thing to ask questions regarding substance misuse, sexual health practices, and COVID-19 safety measures, but through this framework, we were able to take our conversation a step further by asking questions like:
“Walk me through a typical day in your life?” or “How does “x” fit into your day?” and lastly, “What goals do you have for the future?”
Learning how one’s life impacts their health behaviors truly allows us to understand our patients holistically, and in return, be more intentional with the conversations we engage in and the community resources we provide. Once we provided that warm hand-off to the resources our patients needed and followed up after a couple of weeks, we were greeted with a sense of peace knowing that we helped the individual take one step closer to living a healthier life.
One of the greatest takeaways from this fellowship was learning how to fully immerse ourselves in the communities we served. One example of this is asking relevant stakeholders “How can we be helpful?” instead of assuming we know how to be helpful. Lastly, we had the honor to be granted access into the lives of community members, hearing their stories, and offering them encouragement in the face of adversity. One thing we’ve been intentional about (and will continue to be) as future public health professionals and aspiring clinicians is to acknowledge the experiences our patients have faced, while in the same breath, uplifting and praising them for how far they’ve come.

